Published October 2020

Summary
Age-related macular degeneration is one of the biggest causes of sight loss in the UK – yet the only treatment available for the condition involves injections directly into the eye. Many patients are desperate for a less invasive treatment, especially one that doesn’t require hospital visits. Dr Felicity de Cogan and her team have discovered a way to carry drugs across the eye’s protective membranes, moving towards the development of eye drops to treat the disease.
My research is developing a drug delivery mechanism that can get these treatments into the back of the eye without the need for an injection
Dr Felicity de Cogan
Age-related macular degeneration (AMD) is one of the biggest causes of sight loss in the UK, affecting around 600,000 people. The only available treatment for neovascular (‘wet’) AMD involves regular injections of drugs directly into the back of the eye, often for many years. This must be done by an ophthalmologist in a hospital setting, and can be distressing for people needing the treatment.
My research is developing a drug delivery mechanism that can get these treatments into the back of the eye without the need for an injection, ideally in the form of eye drops.

Getting drugs into the eye
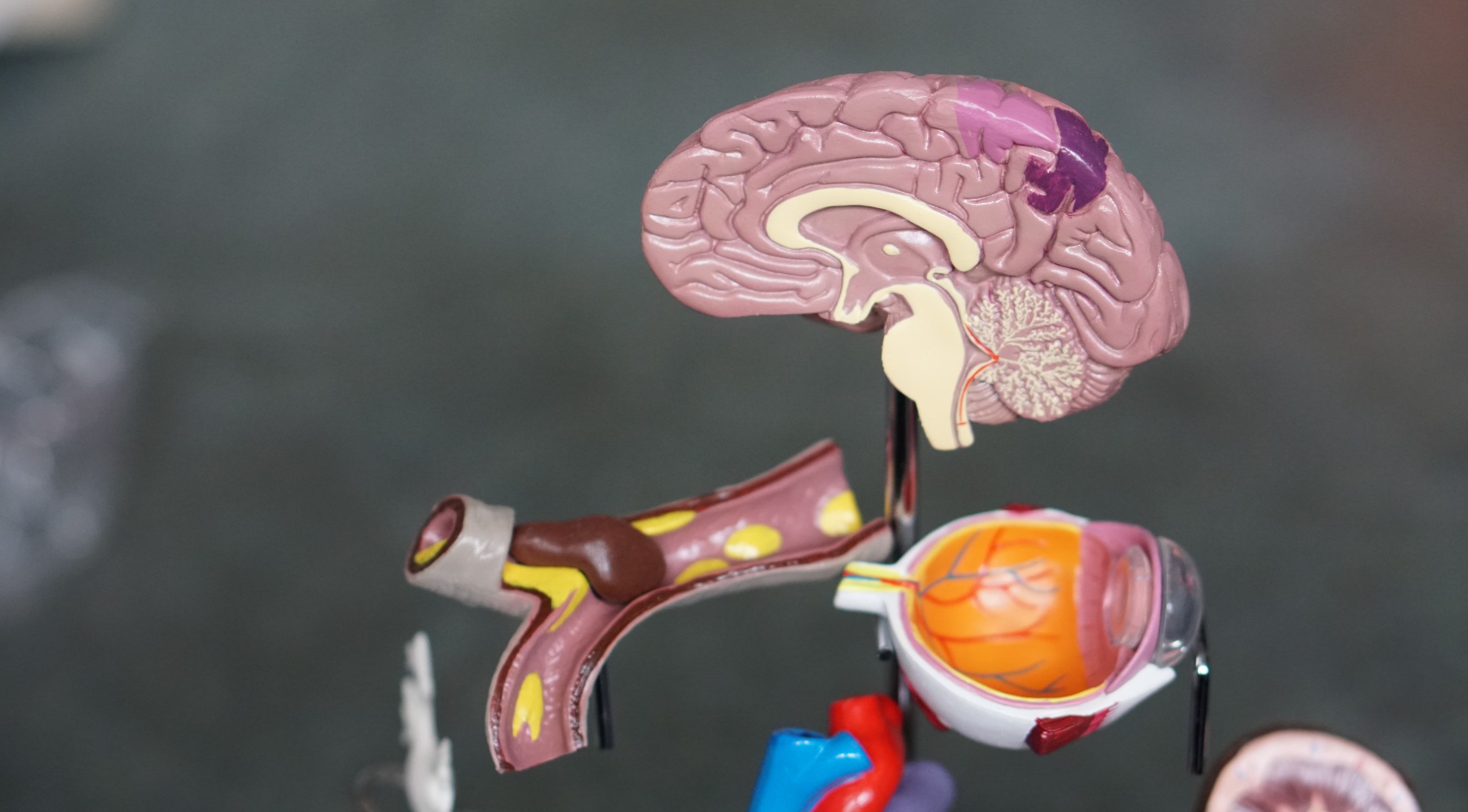
The major hurdle to developing a new AMD treatment is getting drugs into the eye itself. The eye is very efficient at keeping foreign bodies out, and is surrounded by protective membranes. The drugs that we want to deliver to treat AMD are just too big to get across the membranes themselves.
One of the things I’ve tried to do with this project is include patients right from the beginning, asking what they need so we can design therapies that work for them
Dr Felicity de Cogan
To overcome this, we’ve developed a mechanism of carrying drugs across those membranes, known as membrane-penetrating poly-amines (MPPAs). These are molecules that cross the membranes because they are positively charged and can interact with charges on the cell membranes in order to pass through. We can get the MPPAs to act as a ‘cage’ surrounding the drug molecules, carrying them across the membranes.
Making it work for patients
One of the things I’ve tried to do with this project is include patients right from the beginning, asking what they need so we can design therapies that work for them.
Right now we’re looking at dosing regimes. Our patients tell us that it either needs to be a once-a-day or a once-a-month treatment – if it’s something they need to take multiple times a day, or every other day, they’re more likely to forget. At the moment I’m trying to balance how much drug is needed to get into the eye to be effective with how that will actually work with patients’ behaviour.
We’re still working on MPPAs in the lab, and will then move into animal models. By the end of the project, we hope that we’ll get approval to move into clinical trials – providing help for the thousands of people with AMD who are desperate for an alternative treatment.
We’ve experienced some delays to our research as a result of COVID-19, but the Dunhill Medical Trust has been really helpful. What has really stood out from them is that they got in touch with me at the start of the pandemic and said “Just don’t stress about this, our primary concern is supporting our grants and research staff”. I think they were really unique in doing that, and it was a massive relief.