Dementia is a complex condition that can progress rapidly in some people. Professor Kelvin Jordan and Dr Michelle Marshall from Keele University are leading a team of researchers using routinely gathered patient data from GP medical records to find out more about the pathways of progression in dementia, so we can identify people who are most at risk of deteriorating quickly and intervene sooner rather than later.
Around 850,000 people are currently living with dementia in the UK, and the condition varies widely. Some people with dementia get worse rapidly, and quickly need to move to a care home or die early, while others live with it for much longer.
Currently, we don’t have a thorough understanding of the mechanisms behind dementia or the factors that influence its progression. But if we could identify critical markers that suggest a person’s dementia is advancing quickly, it would enable us to manage them more closely and intervene at the right time for how their dementia is progressing.
However, clinical studies aiming to increase our knowledge about dementia often struggle to provide meaningful results on early progression. That’s why we’re turning to routinely collected primary care records to find out more about the early markers of progression in dementia.
Dementia is typically managed in primary care, so these health records tell the stories of which patients have indicators of short-term deterioration and are getting worse quickly. Identifying these people means we can intervene and plan better care for them.
Professor Kelvin Jordan
The MEDDIP study
We recently completed a study in collaboration with the Midlands Partnership NHS Foundation Trust called the MEasurement of Dementia DIsease Progression in Primary care study, or MEDDIP for short. The aim of the study, funded by the Dunhill Medical Trust, was to look for relationships between dementia progression and the kinds of things that GPs and practice nurses routinely record when they see patients, such as symptoms, medications, or changes at home.
During the study we reviewed previous research, analysed anonymised primary care records, and spoke with healthcare professionals, researchers, people with dementia and caregivers to identify potential markers of disease progression. Then we tested how our markers related to other accepted measures of worsening dementia, including assessments conducted in specialist dementia services and outcomes such as hospital admissions or deaths.
Identifying markers of dementia progression
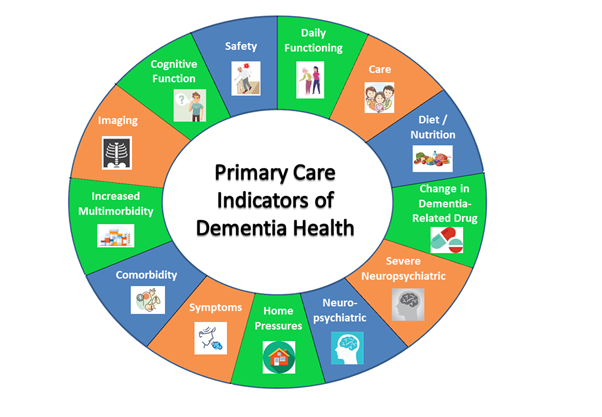
Although we couldn’t find a consistent pattern of disease progression, we identified more than 60 markers associated with deterioration. We grouped these markers into 13 categories, which we presented in a wheel to help patients and clinicians understand the factors associated with worsening dementia.
One of the strengths of the MEDDIP study is that the work can be applied to everybody with dementia, because everyone has a GP. Not everyone with dementia is seen by a specialist service, and we know that access to specialist services varies around the country.
Michelle Marshall
Our study was only possible because we had access to anonymised primary care data to look for patterns and associations between different factors and the speed of dementia progression. It also meant that we could test the accuracy of our markers by looking across anonymised GP data from a representative sample of 30,000 people with dementia in the UK, without burdening them and their carers with the process of a formal clinical study.
A new way to share results
Sharing the results of the study has been a challenge because of the COVID-19 pandemic. We had an event planned for April 2020 with a full list of attendees, but when the pandemic hit we had to cancel. The DMT gave us the time and space to adapt and move our plans online.
To share our key findings, we created an animation aimed at patients and carers and a talking-head video aimed at medical professionals. Patient advocates and their carers helped us craft our resources, so they made sense to them as well as to medical professionals.
What’s next?
Next, we want to dig deeper into the predictive abilities of our markers and use them to create an algorithm that identifies people who are at high risk of rapid deterioration, similar to the existing cardiovascular risk and diabetes risk predictors currently in use by GPs.
MEDDIP was a small study, and it’s these next developments that could have a significant impact. Working with the DMT has been great because they see the importance of supporting smaller studies like MEDDIP, that lay the groundwork for the bigger steps that come next.
Find out more
We have published two papers describing our work on the MEDDIP study in Aging & Mental Health and the European Journal of Neurology. If you want to learn more about the study and its outcomes, you can visit our website, watch our animation or view our talking-head video.
You can also read this blog post, written by Professor Carolyn Chew-Graham for Alzheimer’s Research UK, highlighting the impact and importance of our work on MEDDIP.

