
Published January 2024
Summary
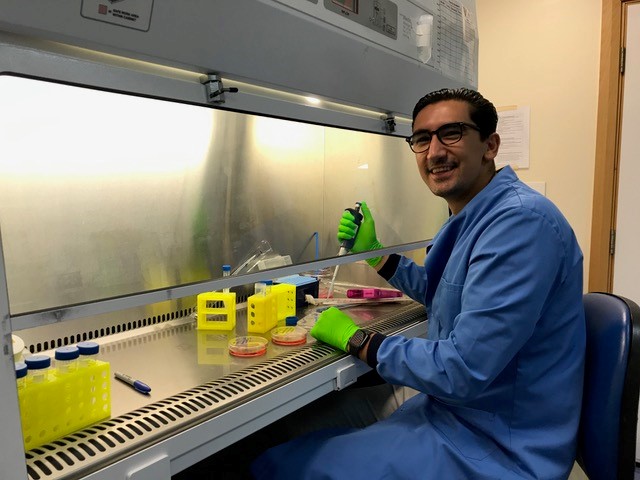
Frozen shoulder is a painful and disabling condition, but how it develops remains a mystery. This motivated Dr Hamez Gacaferi, at the Dakin Group at the University of Oxford, to investigate what drives frozen shoulder and to search for new insights that could lead to better treatments.
We’ve known about frozen shoulder for over 150 years, but we still don’t know what’s driving the underlying inflammation and fibrosis
Dr Hamez Gacaferi
Frozen shoulder, also known as adhesive capsulitis, is a common inflammatory condition that causes scarring in the shoulder joint capsule (fibrosis) leading to pain and immobility. People with frozen shoulder can often be limited in their daily life due to chronic pain.
While frozen shoulder tends to resolve on its own, it can last for up to three years. As well as physical pain, those with frozen shoulder can also experience anxiety, stress and depression, which can linger beyond the lifetime of the condition as people feel uncertain about the future implications of this disease.
Despite frozen shoulder being a common cause of shoulder pain affecting patients between 40-70 years old, the underlying mechanisms behind it remain a mystery. Often older patients with age-related diseases like diabetes mellitus and cardiovascular disease are highly susceptible to developing frozen shoulder. That’s why I wanted to investigate further. We set out to understand how frozen shoulder is triggered and maintained, how it resolves itself and whether there are better ways to treat it.
Letting the data lead the way
We’ve known about frozen shoulder for over 150 years, but we still don’t know what’s driving the underlying inflammation and fibrosis. I had previously studied alarmins – the immune system’s danger signals – in frozen shoulder, back in 2018. But we quickly realised that just focussing on alarmins wasn’t letting us see the bigger picture.
So we generated additional data using single cell RNA sequencing, which gave us very detailed information of what’s going on in frozen shoulder. This data let us identify the cell types, several molecules and pathways involved in this disease – as well as how certain cells were interacting with each other.
A cellular map of frozen shoulder
I believe that we’re merely years away from fully unravelling the puzzle that is frozen shoulder
We created a single cell atlas of the frozen shoulder joint capsule – essentially a map of each cell and how they interact with each other in the shoulder joint. This allowed us to take a look at all the cells present and identify cell populations which play an important role in frozen shoulder.
The largest cell population is made up of fibroblasts, a type of cell that contributes to the formation of connective tissue. In addition, we see macrophages, a type of immune cell involved in inflammation. When we dug deeper, we found that the macrophages and fibroblasts interact with one another.
Communication between these cells seems to be what drives the disease and what helps to resolve it. We identified one pathway in particular, the interleukin 1 axis – known to promote pro-inflammatory signals – which likely drives the inflammation seen in frozen shoulder.
I’m not only grateful that the DMT funded me to explore a disease we don’t fully understand, but also for the immense support I’ve received from them. This funding allowed me to collaborate with an amazing team at the University of Oxford, working with rheumatologists, cell biologists, statisticians, and the clinical team to take a multidisciplinary approach.
Next steps towards a potential treatment
There are options available to treat frozen shoulder – from physiotherapy, steroid injections, painkillers, and surgery. However, because these approaches don’t solve the root cause of the disease, they are often not very effective.
Next steps involve working out exactly what these macrophages and fibroblasts are saying to each other and why, as well as understanding how that changes over time. One way we might be able to treat this disease is to influence how these cells talk to each other with drugs – and therefore get the frozen shoulder to resolve itself faster.
Excitingly, some of the cellular pathways that we have identified so far have already been studied in other joint diseases, such as rheumatoid arthritis. Treatments targeting these pathways have already passed clinical trials – so we could try to use these existing therapies to treat frozen shoulder patients.
I believe that we’re merely years away from fully unravelling the puzzle that is frozen shoulder. Once we get more preclinical data, we can do some further experiments to fully understand which pathways are active in this disease. In the meantime, it’s possible to look at similar diseases which have been studied in more detail. Once we get a clearer picture, we can then move on to see if we can develop treatments that we can use to help patients.

